Assessing and Responding to the Oral Health Care Needs of Adults in a Bleeding Disorders Population
Non-severe hemophilia is not benign? - Insights from the PROBE Study
Characteristics of persons with hemophilia A treated with emicizumab with or without factor VIII inhibitors
Real-world treatment patterns, health outcomes, and healthcare resource use among persons with hemophilia A
Analysis of Bleeding and Treatment Patterns in Children and Adolescents before and after Von Willebrand Disease Diagnosis Using Data from a US Medical Claims Database
Incidence and Prevalence of Diagnosed and Undiagnosed Hemophilia A and Hemophilia B in the USA
A US payer database algorithm to identify clinical profiles of hemophilia B for burden of illness assessment
Von Willebrand Disease: An international Survey to Inform Priorities for New Guidelines
Evaluation of Patient and Physician Reported Reasons for Switching FVIII Replacement Therapies Among Patients With Hemophilia A
Patients Report High Satisfaction with US Hemophilia Treatment Centers: National Trends 2014 and 2017
Satisfaction with Teen Transition Services at US Hemophilia Treatment Centers by Center – Variation by Pediatric and Lifespan Centers 2014 and 2017
An evaluation of health utility and quality-of-life in hemophilia: a systematic literature review
Impact of hemophilia on employment - Insights from the PROBE Study
Identification of Challenges and Coping Strategies in the Management of Bleeding Disorders, From the Patient Perspective
Objective:
We conducted a pilot study using a single open-ended question to elicit patient-perceived challenges and management strategies in individuals with bleeding disorders. The de-identified responses and themes expressed in this study were analyzed. The identification of perceived challenges and management strategies in individuals with bleeding disorders offers the opportunity to improve value based care.
Methods:
This retrospective, cross-sectional cohort study used a sample of convenience at The Hemophilia Center at OHSU. Study population included 20 participants. Inclusion criteria included: ages seven to eighty nine, diagnosed with a bleeding disorder and seen during any outpatient Hemophilia Center clinic visit between March 1, 2017 and April 30, 2018. Participants were included if, during the course of their clinical care, they answered the question, “What is the most significant (or greatest) challenge you have in managing your bleeding disorder and what do you do about it?” Data extracted included question response, age, type and severity of bleeding disorder. Responses were analyzed for themes by the investigators and using qualitative data analysis software. Coded demographic data was correlated.
Summary:
Seven challenge themes were identified: activity restrictions, infusions, emotion/stress, pain, future plans, education and access. Management themes included: self-advocacy, parent directed, activity modification or avoidance, acceptance, inquiry, asking for assistance, planning ahead, resiliency, and peer supports. Younger participants’ (9-17 years) challenges included activity restriction and infusions with management strategies of self-advocacy, activity avoidance and modification. Participants aged 18-57 years highlighted challenges with access to care, infusions, emotion/stress, pain, education and future planning. Management strategies in this group were focused on acceptance, planning ahead, peer support and resiliency. Analysis based on severity of bleeding disorder revealed that subjects with severe hemophilia reported infusions and activity restriction as their most significant challenge, with self-advocacy and activity modification management strategies. Participants with moderate hemophilia reported challenges centered on activity restriction and education of peers, with management strategies being self-advocacy and planning ahead. There were no differences in themes identified when analyzed based on type of bleeding disorder.
Conclusions:
This study characterizes the unique challenges and management strategies described by individuals with bleeding disorders. The themes highlighted the importance of patient voice and can be used to inform individual care decisions.
Patient Satisfaction with US Hemophilia Treatment Centers: National Trends 2017
Objective:
Patient satisfaction with healthcare services is a measure of patient centeredness, influences treatment adherence, and increasingly affects reimbursement. In 2018, the US Hemophilia Treatment Center Network (USHTCN) launched the second national Patient Satisfaction Survey (PSS).
Methods:
A Steering Committee and Regional HTC Coordinator work group updated, piloted, and finalized the two-page survey for patient self-administration online, at clinic, or at home, in English or Spanish, and mailed to households. Survey content and format were based on national health surveys to enhance comparability and scientific robustness. Questions included assessed patient demographics, satisfaction with team members, and care processes aligned with HRSA goals. An open ended question sought qualitative data. Respondents were anonymous but the HTC where they received care was identified. Participation was voluntary. Persons with genetic bleeding disorders who had HTC contact in 2017 were eligible. Since March 2018, HTCs sent surveys to approximately 31,650 households. Parents were asked to complete surveys for children under age 15. No reminders were sent. Data were entered and analyzed at a central site and aggregated at national, regional and HTC levels. Survey remains open through summer 2018.
Results:
4042 individuals (12.8%) from 125 (90%) of the 139 Centers in the USHTCN returned surveys by June 12, 2018. National analyses on 4042 surveys reveal that 93% - 98% were ‘always’ or ‘usually’ satisfied with HTC care processes: shared decision making (97%); care coordination (97%); obtaining understandable information (97%); getting timely services (95%); enough time with staff (97%); being treated respectfully (98%); and HTC Factor Program/Pharmacy (340b) (96%). 95% - 97% were ‘always’ or ‘usually’ satisfied with core HTC team members. 91% of 12-17 year olds were ‘always’ or ‘usually’ satisfied with HTC encouragement regarding becoming more independent, and 92% with how the HTC discussed caring for a bleeding disorder upon reaching adulthood. Insurance and language were ‘always’ or ‘usually’ a problem for 14% and 9% respectively. 31% of respondents were female and 10% Hispanic. 80% were Caucasian, 5% African-American, 4% Asian/Pacific Islander or Native Hawaiian, 4% Multiple races, and 7% did not respond. Over 60% had severe or moderate FVIII or FIX deficiency or VWD Type 3. Ages ranged from newborns to over 90 years: 37% under 18, 18% age 18 – 34, and 45% over age 35.
Conclusions:
Implementing a National Patient Satisfaction Survey for the USHTCN remains feasible, is supported by HTCs nationally, and provides valuable information. Satisfaction with HTC services including 340B pharmacy is high. Insurance and language pose problems for 9-14%. Future analyses will examine additional national data and regional variation, and identify trends from the first national PSS conducted in 2014.
Living with hemophilia B: examining quality of life and associated characteristics in the Hemophilia Utilization Group Studies (HUGS Vb) cohort
What Symptoms of Hemophilia Most Impact Quality of Life – A Quantitative Survey of People Living with or Caring for Someone with Hemophilia A
Lessons Learned in the Assessment of Functional Status in US Adults With Hemophilia in the Pain, Functional Impairment, and Quality of Life (P-FiQ) Study: Importance of More Formalized Assessment of Function in the Comprehensive Care Setting
Objective:
Functional impairment from recurrent joint bleeding in people with hemophilia results in joint pain and reduces quality of life. The P-FiQ study formally evaluated patient- and site-reported functional assessment including responses to generic and hemophilia-specific patient-reported outcomes (PROs) tools. Psychometric analyses were used to evaluate reliability, validity, and consistency of responses.
Methods:
Adult males with hemophilia and a history of joint pain or bleeding completed a hemophilia history and 5 PROs assessing function: EQ-5D-5L, Brief Pain Inventory v2 Short Form (BPI), International Physical Activity Questionnaire (IPAQ), Short Form-36 v2 (SF-36v2), and Hemophilia Activities List (HAL). PROs were assessed for reliability, consistency, and correlation, with factors including patient-reported characteristics.
Summary:
A total of 381 adults (median age, 34 years; range, 18-86 years) were enrolled in P-FiQ. Most participants (66%) and sites (59%) reported functional disability in the past 6 months (CDC-UDC scale). Patients self-reported arthritis/bone/joint problems (65%) and history of joint procedures or surgeries (50%). On EQ-5D-5L, most reported problems “today” with mobility (61%) and usual activities (53%) but fewer with self-care (19%). On BPI, similar median pain interference scores (0- 10 scale, 10 is complete interference) were reported with general activity (3.0), walking ability (3.0), and normal work (3.0). On IPAQ, physical activity was reported by 49% of respondents over the prior week, with more reporting walking (35%) than moderate (16%) or vigorous (16%) activities. On SF-36v2, activities in the past 4 weeks that were most frequently limited were vigorous activities (80%), bending, kneeling, or stooping (67%), walking more than a mile (61%), and climbing several flights of stairs (59%). Physical problems caused participants to limit kinds of work/activities (69%), accomplish less than they would like (66%), have difficulty in performing work/activities (65%), and reduce time spent on work/activities (62%). On HAL, greater difficulties were seen for lower vs upper extremity functions/activities; within the lying/sitting/kneeling/standing domain, the most frequent problems in the previous month were squatting for a long time (74%), kneeling (73%) or standing (72%), and kneeling/squatting (70%). Similar items across different PROs were correlated with one another. Self- reported functional impairment was significantly differentiated by BPI pain interference, IPAQ total activity, SF-36v2 physical functioning, and all HAL domains and summary scores.
Conclusion:
PRO instruments assessing functional status range from simple/generic (EQ-5D-5L) to complex/disease-specific (HAL) and provide varying levels of detail. Greater use of formal PRO instruments in the clinical setting may improve dialogue between health care professionals and patients/caregivers and inform proactive approaches to specifically target patient identified functional limitations (eg, HAL) and identify areas for further targeted management strategies.
Lessons Learned From the Assessment and Prevalence of Anxiety and Depression in US Adults With Hemophilia in the Pain, Functional Impairment, and Quality of Life (P-FiQ) Study: Importance of Routine Screening and Comprehensive Approaches to Management
Lessons Learned in the Assessment of Pain in US Adults With Hemophilia in the Pain, Functional Impairment, and Quality of Life (P-FiQ) Study: Importance of More Formalized Discussions Around Pain in the Comprehensive Care Setting
Objective:
People with hemophilia frequently experience joint bleeds, resulting in pain and functional impairment. The P-FiQ study formally evaluated patient-reported pain descriptions, responses to standardized patient-reported outcomes (PROs) related to pain, and pain management strategies.
Methods:
Participants completed a pain/hemophilia history and 5 PRO instruments. Pain was assessed via 3 PRO instruments: EQ-5D-5L, Brief Pain Inventory v2 Short Form (BPI), and Short Form-36 v2 (SF- 36v2), and these instruments were assessed for reliability, consistency, and correlation with factors including patient-reported characteristics.
Summary:
P-FiQ enrolled 381 adult males with mild-severe hemophilia and a history of pain and/or joint bleeding. Most (65%) self-reported having arthritis/bone/joint problems. Thirty-two percent of participants reported experiencing both acute and chronic pain, 35% chronic pain only, 20% acute pain only, and 15% no pain. Of those reporting acute pain, most described the sensation as “sharp” (77%) or “aching” (65%); for those reporting chronic pain, most described the pain as “aching” (80%) or “nagging” (50%). Ankles (37%) and knees (24%) were commonly reported as the most painful joints. Many participants with acute/chronic pain reported using acetaminophen (62%/55%) or nonsteroidal anti-inflammatory drugs (34%/49%) to treat their pain in the past 6 months. Some participants indicated having moderate/severe/extreme (28%/12%/2%) pain/discomfort “today” as measured by the EQ-5D-5L pain/discomfort domain. For BPI (scale 0-10, 10 is most severe pain), median pain severity scores were 6.0 for worst pain, 3.0 for average pain, 2.0 for current pain, and 1.0 for least pain. Median BPI pain interference scores indicated interference with general activity (3.0), mood (3.0), walking ability (3.0), normal work (3.0), and enjoyment of life (2.0). On SF-36, most participants (90%) reported experiencing bodily pain, and 75% indicated that pain interfered with normal work in the last 4 weeks. Assessments of pain on PROs were highly correlated with one another. The following formal PRO assessments were associated with self-reported pain: pain/discomfort domain of EQ-5D-5L, BPI worst pain, least pain, average pain, and current pain, and SF-36 bodily pain. Greater extent of lifetime routine infusions was also associated with EQ-5D-5L pain/discomfort and SF-36 bodily pain.
Conclusion:
Pain severity and interference in people with hemophilia were identified consistently across several PROs, and correlated with patient-reported pain. In the comprehensive care setting, greater use of formalized assessment tools over time would improve dialogue and pain assessment between healthcare professionals and patients, document and validate the presence and extent of pain, establish and monitor individual goals for pain management interventions, and encourage the exploration of various pain management strategies and the evaluation of their overall quality and effectiveness.
IMPACT QoL II - The relationship of depression and anxiety to control of chronic pain and adherence to clotting-factor treatment
Effect of hemophilia treatment center monitoring on bleeding rates
SPACE (Study of Prophylaxis ACtivity, and Effectiveness): An interim descriptive analysis of patient activity levels and participation
Objective:
Personalizing treatment to a patient’s lifestyle and promoting overall health and wellness in persons with hemophilia (PWH) is essential to optimizing outcomes. There is limited evidence that correlates how activity and infusions impact bleeding episodes and further data on this relationship is needed. The research objective of SPACE is to prospectively explore the association between activity level, timing of infusion, and occurrence of a bleeding episode in PWH using novel technology.
Methods:
This six-month prospective, observational study includes PWH A or B in the United States currently receiving ADVATE or RIXUBIS between the ages of 13 and 65 years. Enrolled PWH use a smartphone eDiary application to log information on activities, infusions, and bleeding episodes. As an additional measurement of activity, enrollees are given a FitBit, a consumer-based activity tracker that measures steps taken and calories burned. Activity types are assessed based on their level of perceived risk for collision, according to the NHF “Playing It Safe” brochure. We report here current study status and descriptive analysis of baseline data.
Results:
The interim analysis included 15 patients with a median age of 19 (Range: 13 to 47). At baseline, 87% of patients were on prophylaxis and 13% treated on-demand treatment. Fifty-three percent of patients had 0 target joints at baseline. Eighty-seven percent of patients indicated that they had discussed activity participation with their physician. Sixty-seven percent of patients considered themselves ‘very satisfied’ or ‘satisfied’ with their level of activity. Data collected from the FitBit indicated that patients in SPACE walked on average 7,367 (SD: 3250) steps per day and burned 979 (SD: 398) calories from their activity. For patients on prophylaxis, the mean number of days per week doing mild, moderate and strenuous activity were 3.57, 2.64, and 1.5 respectively. Of the data reported on bleeding episodes, 40% of patients reported no bleeds at the time of the interim analysis. Forty percent of patients did not report having a bleed at the time of the interim analysis. Of all bleeds reported, 34% were associated with physical activity.
Conclusions:
Current data from SPACE demonstrates that subjects are active and participating in various activities. Continued data will provide better understanding of the types of activities and infusion schedules that may be associated with risk as well as protective effects on bleeding episodes by infusing prior to activity. A personalized approach to treatment based on physical activity levels may minimize bleeding risk in PWH.
Hemophilia B Patients Who Switch From rFIX to Extended Half-Life rFIX-Fc: A Retrospective Analysis of Cost using US Specialty Pharmacy Dispensing Data
Initial Observations From the Pain, Functional Impairment, and Quality of Life (P-FiQ) Study: Patient-Reported Outcome Assessments in US Adults With Hemophilia
Development of a novel patient-centered outcome measure in hemophilia using Goal Attainment Scaling
Background and Objective:
Standard outcome measures in hemophilia, such as the annual bleeding rate, have inherent limitations in both clinical practice and in research, including lack of both sensitivity and personalization. Goal attainment scaling (GAS) is a method for evaluating outcome that is patient-centered and sensitive to change in individuals and populations; collaborative goal setting may also be viewed through the biopsychosocial lens as a potential resource to strengthen disease-related coping. GAS has been used successfully in several disease areas. However, feasibility can be an issue. To address this, standardized goal attainment menus can be developed that preserve individualization, while allowing greater ease of use by non-experts. We initiated a process to develop a novel outcome measure in hemophilia, the GAS-Hem, by creating a goal attainment menu for patients living with hemophilia.
Methods:
We conducted 2 multidisciplinary workshops with participants from medicine, nursing, social work, and physical therapy (n=12). During the first workshop, we developed a list of goal areas, each with an associated set of descriptors of attainment levels. At the second workshop, a second group of experts (n=8) critically reviewed each goal to evaluate its importance and relevance for inclusion in the GAS-Hem.
Summary:
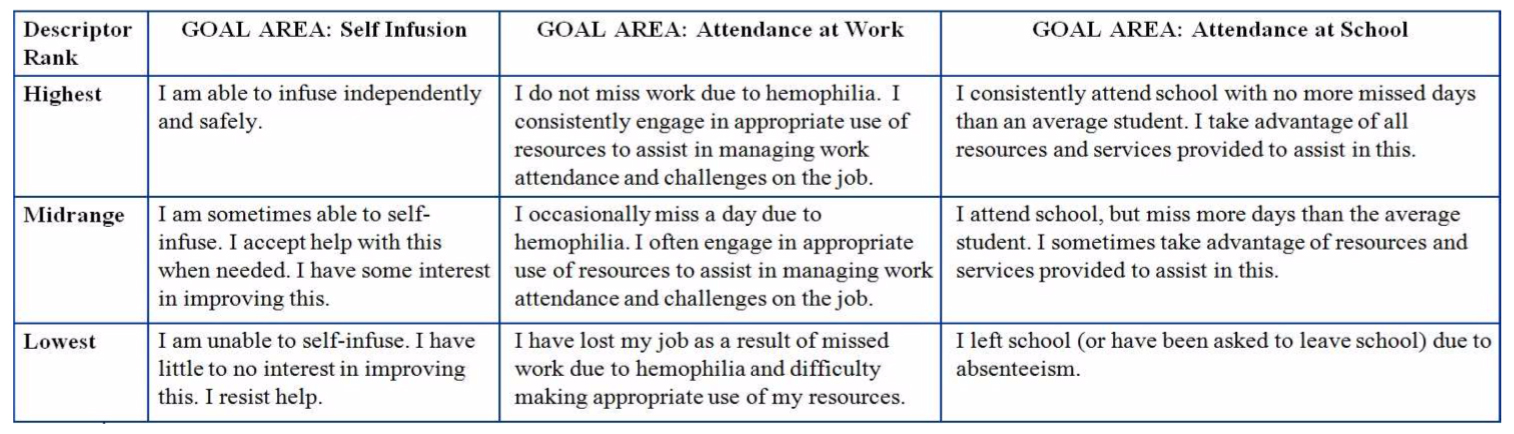
28 goal areas with associated descriptors of attainment levels were developed, covering 3 broad categories: ability to manage hemophilia, ability to recognize and treat complications, and ability to cope with the impact of hemophilia on daily life. Descriptors incorporated several key parameters for each goal (eg. skill level, desire for change, utilization of available resources) (Table).
Conclusions:
We developed a novel, patient- centered outcome measure for patients with hemophilia. A comprehensive, preliminary list of goal areas and attainment levels was successfully created. The next step will be to incorporate feedback from patients and families, after which a feasibility study will be conducted to evaluate content and construct validity and overall ease of use.
Table. Examples of Goal Areas and Descriptors
Description and Management of Pain and Functional Impairment in US Adults With Hemophilia: Initial Observations From the Pain, Functional Impairment, and Quality of Life (P-FiQ) Study
Global Knowledge and Confidence Assessment of Hemophilia Clinical Practice Approaches Among Pediatricians
Objective:
Clinical knowledge gaps of hemophilia can affect patient outcomes through delayed diagnosis/referral as well as improper monitoring and interventions. A study was undertaken to identify and characterize clinical practice gaps and confidence levels in the management of hemophilia specific to pediatricians.
Methods:
Building upon a previous assessment developed in 2014, an updated global, hemophilia-specific continuing medical education-accredited clinical practice assessment survey was developed utilizing current evidence-based consensus guidelines and best practices, including guidelines from the National Hemophilia Foundation and the World Federation of Hemophilia. The assessment included both knowledge- and case -based, multiple-choice questions that healthcare providers completed confidentially on-line between March 23, 2015 and April 9, 2015. Areas such as appropriate triggers for initiating prophylaxis and use of physical therapy were assessed. Responses from pediatric providers were de- identified and aggregated prior to analysis.
Summary:
660 pediatricians (30% of total respondents) completed the survey, from the following locales: North America (36%), Asia (23%), Europe (15%), Middle East (10%), Africa (7%), Central/South America (6%), and Australia (4%). Academic (31%), private practice (27%), community hospital (19%), community clinic (12%), and hemophilia treatment center (3%) practice settings were identified. Analysis of pediatricians who indicated professional interaction with hemophilia patients (87% of pediatrician respondents) demonstrated knowledge gaps including (% incorrect responses): classification of severity of hemophilia (37%); optimal use of prophylactic therapy, e.g., when to initiate (31%), at what dose (53%), prophylaxis in active patients (26%); likelihood of inhibitors (75%); using bypassing therapy (58%); comprehensive care model (61%); supporting overall joint health and quality of life (70%); and adherence (60%). A low level of confidence in the ability to identify when to use prophylaxis was reported among 31% of pediatricians. The top barriers to the administration of prophylaxis identified by the pediatric providers included lack of availability of FVIII or FIX concentrates, lack of venous access, and insurance coverage (29%, 22%, and 21% for respondents, respectively).
Conclusions:
This study demonstrated gaps in knowledge and confidence about the assessment and optimal care of hemophilia for pediatricians, suggesting that further education specific to the needs of these providers is warranted.
Associations Between Annual Bleeding Episodes and Financial Burden of Illness Among Persons with Hemophilia A and B in the United States
Patient Satisfaction with US Hemophilia Treatment Centers 2015: National Results
Objective:
Patient satisfaction with healthcare services enhances patient experience, improves outcomes, and is increasingly mandated by public and private payers. While many US Hemophilia Treatment Centers (HTC) periodically assess patient satisfaction, the lack of a uniform survey hampered national measurement. To remedy this knowledge gap, the US HTC Network implemented a national patient satisfaction survey in 2015.
Methods:
A Regional HTC Coordinator workgroup devised, piloted, and finalized a two-page survey for self-administration online, at clinic, or at home, in English or Spanish and mailed to households. Survey content and format were based on national health surveys to enhance comparability and scientific robustness, informed by legacy regional HTC surveys. Questions assessed patient demographics; satisfaction with services, team members, and care processes; and Healthy People 2020 adolescent transition objectives. Surveys included open ended questions to obtain qualitative data. Respondents were anonymous but identified with their respective HTCs. Participation was voluntary. Persons with genetic bleeding disorders who had HTC contact in 2014 were eligible. During February 2015, 124/130 HTCs sent surveys to 27,563 households. Parents completed surveys for children under age 15. No reminders were sent. Data were entered and analyzed at a central site and aggregated at national, regional and HTC levels.
Results:
Over 4800 households (17.4%) returned surveys by April 30, 2015. National analyses on 4332 surveys reveal that 96.6% were ‘always’ or ‘usually’ satisfied with HTC care. Over 80% were ‘always’ satisfied with the core HTC team members. Three quarters of 12-17 year olds were ‘always’ satisfied with HTC encouragement regarding becoming more independent, and how the HTC discussed caring for a bleeding disorder upon reaching adulthood. Eighty– 90% were ‘always’ or ‘usually’ satisfied with care processes, e.g. shared decision making, care coordination, ease of obtaining timely information and services, and being treated respectfully. Insurance and language were ‘always’ a problem for 20%. 29.0% of respondents were female and 10.3% Hispanic. 83.4% were Caucasian, 5.8 African- American, 3.1% Asian/Pacific Islander or Native Hawaiian, 4.3% Multiple races, and 4% Other. Over half had severe or moderate FVIII or FIX deficiency or VWD Type 3. Ages ranged from newborns to 96 years: 38% under 18, 20% age 18 – 34, and 42% over age 35.
Conclusions:
Implementing a National Patient Satisfaction Survey for the US HTCN is feasible, and provides valuable information. Satisfaction with HTC services is high, but insurance and language ‘always’ pose problems for one fifth. Further analyses will examine regional differences.

